Perivascular epithelioid cell tumor of male pelvic cavity: a case report and literature review
Abstract: Perivascular epithelioid cell tumors (PEComas) are a family of rare mesenchymal neoplasms. The PEComas, composed of epithelioid and spindle cells, have the same cellular and immunohistochemical features but are found in different visceral and soft tissue sites. Here, we report the histological and immunohistochemical features of one case of PEComa restricted in the pelvic visceral peritoneum of a male patient. The patient was treated with radical surgery, and was well and on follow-up visits without tumor recurrence.
Key words: Perivascular epithelioid cell tumor; pelvic cavity; surgical resection; treatment
Introduction
Perivascular epithelioid cell tumors (PEComas) are a rare group of mesenchymal neoplasms and are predominantly composed of eosinophilic epithelioid cells, with typically morphological, immunohistochemical (IHC) and molecular findings.
PEComa has been described in many locations, involving digestive system, kidney, lung, soft tissues, female genital tract organs and so on (1). The tumor can be most commonly seen in the uterus. Nevertheless, Pan (2) had reported one case of PEComa arising in male prostate, Gronchi (3) had reported one case of angiomyolipoma arising in the pouch of Douglas, and Kim (4) had reported one case of lymphangiomatosis arising in a woman’s pelvic cavity. Here, we present a case of PEComa of visceral peritoneum located in the pelvic cavity of a male patient.
Case report
On November 2010, a 23-year-old man was admitted to hospital for the tumor in pelvic cavity which was occasionally found during the annual health check. The patient, without clinical or family history, had no distinctive symptoms or signs. Hematological and chemical studies, including tumor markers, exhibited normal results. A computerized tomography (CT) scan showed a well demarcated round mass in the right pelvic cavity. The tumor, as a well delimited nodule located in the pelvic visceral peritoneum closing to the bladder, was 8 cm × 6 cm, and completely resected. There was no evidence of the disease elsewhere. Hence, the tumor was regarded as a primary pelvic visceral peritoneum tumor. The patient was treated exclusively with surgical resection and was well during the follow-up period. There was no evidence of tumor recurrence or metastasis.
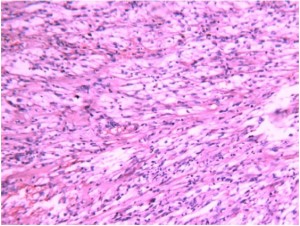
The tumor was 6.5 cm × 5.0 cm × 4.5 cm, and well circumscribed but not encapsulated. The cut surface of the tumor was brown-reddish with elasticity. Microscopic examination revealed that the neoplasm was predominantly composed of epithelioid and spindle cells. The spindle cells mainly located in the center area of the tumor while the epithelioid cells mainly located in the marginal area. The spindle cells, resembling smooth muscle cells, tended to have abundant clear cytoplasms and arranged in a storiform shape. The epithelioid cells, having abundant clear eosinophilic cytoplasms and apparent nucleoli, were mostly arranged as small nests commonly related to variably-sized vessels. There was no necrosis, angiolymphatic invasion or perineural infiltration, and the mitotic index was low (<1/50HPF). There was no adipose tissue in the tumor (Figure 1).
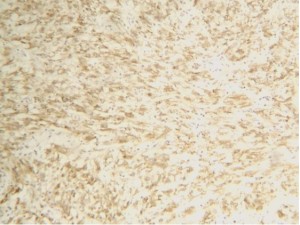
The tissue obtained at the time of surgery was fixed in 10% buffered formalin and routinely paraffin-embedded. Tissue sections were stained with hematoxylin-eosin (HE). The IHC analysis was carried out on paraffin sections using Non-Biotin HRP Detection System (BioGenex Laboratories, CA, USA). The primary antibodies included the antibodies against melanoma (HMB45), Melan A, S-100 protein, smooth muscle actin (SMA), CD34, CD117, synaptophysin (Syn) and chromogranin A (CgA), respectively. All the primary antibodies were bought from Zhongshan Goldenbridge Biotechnology Co., LTD (Beijing, China). The IHC results showed that the tumor cells were positive for HMB45, Melan-A and SMA, but negative for Syn, CgA, CD34, CD117 and S-100 (Figure 2).
The slices including HE and IHC staining were also interviewed by doctors of The First Affiliated Hospital of Zhejiang University and the same result was given. The patient was followed up till now.
Discussion
PEComa is a rare mesenchymal neoplasm. It was first suggested as perivascular epithelioid cell (PEC) in 1996, and was defined by the World Health Organization (WHO) as a mesenchymal tumor composed of histologically and immunohistochemically distinctive PECs in 2002 (5).
The PEComa family is now composed of epithelioid angiomyolipoma, clear cell ‘sugar’ tumor, lymphangioleiomyomatosis, clear cell myomelanocytic tumor of the falciform ligament/ligamentum teres and rare clear-cell tumors of other anatomical sites (6). PEComa is mainly composed of eosinophilic and clear epithelioid cells, which were commonly arranged as small nests related to variably-sized vessels. The tumor cells express melanocytic (HMB45 and/or Melan-A) and smooth muscle (actin and/or desmin) markers (7). In our case, the neoplasm was predominantly composed of epithelioid and spindle cells. The epithelioid cells, having abundant clear eosinophilic cytoplasms, were mostly arranged as small nests commonly related to variably-sized vessels. And the tumor cells were positive for HMB45, Melan-A and SMA. So the pathological findings were consistent with those of PEComa and the IHC findings confirmed the diagnosis.
The main differential diagnosis includes stromal tumor and smooth muscle tumor. Stromal tumor is a common primary mesenchymal neoplasm, but rarely shows oncocytic morphology, clear cell features or pleomorphism. The morphology of leiomyoma and leiomyosarcoma may be very similar to that of PEComa, so the IHC analysis is the only way to establish the diagnosis of PEComa. It is hard to define the biological behavior of PEComa. Some of the patients showed metastasis, recurrence or even post-operational death. So some experts (8) proposed that the disease could be classified into three subgroups, including benign, uncertain malignant potential, and malignant. The benign tumors have no malignant features (e.g. diameter of the tumor ≤5 cm, non-infiltrative, non-high nuclear grade, mitotic rate ≤1/50 high power fields), while the uncertain malignant potential tumors show pleomorphic or multinucleated giant cells only, or sized over 5 cm in diameter only. But the tumors should be regarded as malignant if they exhibit infiltrative growth, high mitotic activity, atypical mitotic figures and coagulative necrosis. Bosincu (9) reported two cases of aggressive PEComa and one patient died at one year after diagnosis. On the cut sections of the two cases, necrotic and hemorrhagic areas and myometrial infiltration were seen. Among four cases of PEComa reported by Bonetti (10), two cases showed myometrial infiltration and enlarged lymph nodes and were finally diagnosed as malignant PEComa. To date, only two cases of primary fibular PEComa were reported, and one case reported by Lian (11) was finally diagnosed as malignant PEComa, because it exhibited bone and soft tissue infiltration, necrosis, vascular invasion and high mitotic index. Although rare malignant cases have been reported (9-13), most of these tumors are benign or of uncertain malignant potential (14-17). In our case, the tumor sized over 5 cm in diameter, but it did not display infiltrative growth, nuclear enlargement, hyperchromasia, high mitotic activity (the mitotic rate was low, <1/50 high power fields), atypical mitotic figures and coagulative necrosis. So we think this case should be classified to the uncertain malignant potential group.
It is difficult to diagnose PEComa because of its rarity and no distinctive symptoms and signs, so the diagnosis should depend on pathological examinations. Today, radical removal of the tumor is the main treatment method for primary tumor, local recurrence and metastasis. Reports of additional adjuvant treatment do not exist. In the near future, perhaps new specific targeted therapy may be used in patients with locally advanced or metastatic disease. Since PEComa can behave in an aggressive manner, careful follow up is recommended.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Martignoni G, Pea M, Reghellin D, et al. PEComas: the past, the present and the future. Virchows Arch 2008;452:119-32.
- Pan CC, Yang AH, Chiang H. Malignant perivascular epithelioid cell tumor involving the prostate. Arch Pathol Lab Med 2003;127:E96-8.
- Gronchi A, Diment J, Colecchia M, et al. Atypical pleomorphic epithelioid angiomyolipoma localized to the pelvis: a case report and review of the literature. Histopathology 2004;44:292-5.
- Kim HS, Park MI, Suh KS. Lymphangiomyomatosis arising in the pelvic cavity: a case report. J Korean Med Sci 2005;20:904-7.
- Qu GM, Hu JC, Cai L, et al. Perivascular epithelioid cell tumor of the cecum: a case report and review of literatures. Chin Med J (Engl) 2009;122:1713-5.
- Vijayabhaskar R, Mehta SS, Deodhar KK, et al. PEComa of the lung. J Cancer Res Ther 2010;6:109-11.
- Choi CW, Kim TO, Kim KY, et al. Perivascular epithelioid cell tumor (PEComa) of abdominal cavity from falciform ligament: a case report. J Korean Med Sci 2009;24:346-9.
- Gan MF, Yu CK, Jin M, et al. Perivascular epithelioid cell tumor of the uterus: report of three cases. Chin Med J (Engl) 2007;120:526-8.
- Bosincu L, Rocca PC, Martignoni G, et al. Perivascular epithelioid cell (PEC) tumors of the uterus: a clinicopathologic study of two cases with aggressive features. Mod Pathol 2005;18:1336-42.
- Bonetti F, Martignoni G, Colato C, et al. Abdominopelvic sarcoma of perivascular epithelioid cells. Report of four cases in young women, one with tuberous sclerosis. Mod Pathol 2001;14:563-8.
- Lian DW, Chuah KL, Cheng MH, et al. Malignant perivascular epithelioid cell tumour of the fibula: a report and a short review of bone perivascular epithelioid cell tumour. J Clin Pathol 2008;61:1127-9.
- Armah HB, Parwani AV. Malignant perivascular epithelioid cell tumor (PEComa) of the uterus with late renal and pulmonary metastases: a case report with review of the literature. Diagn Pathol 2007;2:45.
- Selvaggi F, Risio D, Claudi R, et al. Malignant PEComa: a case report with emphasis on clinical and morphological criteria. BMC Surg 2011;11:3.
- Zemet R, Mazeh H, Neuman T, et al. Asymptomatic pancreatic perivascular epithelial cell tumor (PEComa) in a male patient: report and literature review. JOP 2011;12:55-8.
- Bradshaw MJ, Folpe AL, Croghan GA. Perivascular epithelioid cell neoplasm of the uterine cervix: an unusual tumor in an unusual location. Rare Tumors 2010;2:e56.
- Zarbis N, Barth TF, Blumstein NM, et al. Pecoma of the lung: a benign tumor with extensive 18F-2-deoxy-D-glucose uptake. Interact Cardiovasc Thorac Surg 2007;6:676-8.
- Freeman HJ, Webber DL. Perivascular epithelioid cell neoplasm of the colon. World J Gastrointest Oncol 2010;2:205-8.