Evolution of viral RNA in a Chinese patient to interferon/ribavirin therapy for hepatitis C
Objective: The combination of interferon (IFN) and ribavirin (RBV) is the standard therapy for hepatitis C
virus (HCV) infection. HCV genotype 2a has proved more amenable to the therapy, but its efficacy is yet limited.
This study aimed to investigate the mechanism of the poor response in a case of HCV genotype 2a infection.
Methods: We analyzed dynamic change of HCV RNA from a patient, infected with HCV genotype 2a,
showing a poor virological response to IFN/RBV as judged 12 weeks after initiation of the therapy by HCV
clone sequencing. Then we constructed subgenomic Japanese fulminant hepatitis-1 (JFH1) replicon and
different chimeric replicons with humanized Gaussia luciferase gene. The chimeric replicons were derived from
subgenomic JFH1 replicon, in which the NS5A region was replaced by the patient’s sequence from the pre/posttreatment,
and the chimeric replicons’ susceptibility to IFN were evaluated by relative Gausia Luciferase activity.
Results: The pretreatment HCV sequences appeared almost uniform, and the quasispecies variation
was further more simplified after 12 weeks of therapy. Besides, the quasispecies variation seemed to be
more diversified in the NS5A, relatively, a region crucial for IFN response, and each of chimeric replicons
exhibited distinct response to IFN.
Conclusions: During the course of the chronic infection, HCV population seems to be adapted to the
patient’s immunological system, and further to be selected by combination of IFN/RBV therapy, indicating
quasispecies may completely eliminated by addition of other drugs with targets different from those of IFN. In
addition, each different response of chimeric replicon to IFN is most likely related to amino acid changes in or
near the IFN-sensitivity determining region (ISDR) of NS5A during chronic infection and IFN/RBV therapy.
Key words: HCV-2a; IFN; poor response; JFH1; chimeric replicon
Introduction
Hepatitis C virus (HCV) is a single stranded RNA virus of positive polarity belonging to the Flaviviridae family. The about 9.6 kb single-stranded viral RNA genome expresses a single polyprotein consisting of about 3,000 amino acids, which undergoes proteolytic cleavage with the help of host and virally-encoded proteases. This results in production of up to 10 different viral proteins, both structural and non-structural (NS) proteins.
HCV infection affects 170 million people worldwide (1). It is estimated that 20% of HCV-infected patients will develop cirrhosis, with the associated risks of developing liver failure and/or liver cancer (2,3). The primary aim of anti-HCV therapy is permanent eradication of the virus or a sustained viral response, finally to prevent development of cirrhosis and hepatocellular carcinoma. Currently, the standard therapy for chronic HCV infection is the combination of pegylated interferon (PEG-IFN) α-2a or α-2b and ribavirin (RBV). The combination of both drugs has a significant effect on virological and histological responses, especially to the patient with HCV genotypes 2, reaching a sustained viral response rate in 80% of patients in randomized controlled trials (4-6).
However, even with genotype 2 HCV infection, the combination therapy for 24 weeks failed to eradicate the virus in about 20% of patients, although the reason is still unclear. To investigate the mechanism of poor response in a case of genotype 2a, we analyzed the HCV RNA sequences before and after standard therapy.
Materials and methods
Patient
One patient chronically infected with HCV-2a, enrolled in HCV clinical trial at Beijing Ditan Hospital, whose diagnosis had been made based on anti-HCV antibody detection, HCV genotype determination according to the method by Okamoto et al. (7) and clinical follow-up, was treated with PEG-IFN-2b (1.5 µg/kg body weight, once a week, subcutaneously) and RBV (600-800 mg daily, per os), according to a standard treatment protocol. The patient was confirmed negative for hepatitis B surface antigen and human immunodeficiency virus (HIV). Plasma samples were collected from the patient during and after 12 weeks of treatment. The quantification of serum HCV RNA titers was performed by reverse transcription-polymerase chain reaction (RT-PCR) with an internal RNA standard derived from the 5' noncoding region of HCV (Amplicor HCV Monitor test, version 2.0, Roche Diagnostics, Tokyo, Japan). The viral load before treatment (0 week) and during treatment (12 weeks) is 1.95×107 and 2.19×103 IU/mL, respectively.
The study protocol was approved by the Ethic Committee of Beijing Ditan Hospital, and written informed consent was obtained from the patient before the treatment.
Sequence analysis
RNA was extracted from 150 µL of plasma with ISOGEN-LS (Wako Corporation, Japan). For amplification of different region of the HCV genome, covering NS4B, NS5A and NS5B, the extracted RNA was reverse-transcribed and amplified using PrimeSTAR Max DNA polymerase (Takara Bio Inc., Japan). The sets of primers are: 8S [5’-AAACACATGTGGAACTTCATC-3'; sense nucleotide (nt) 5,639-5,659] with 8As (5'-GGAT GGATCTGTTAGCATGGAC-3'; sense nt 6,868-6,889), 9S (5'-ACTGGTATCATGACCACACG-3'; sense nt 6,416-6,435) with 9As (5'-GCGTCCTGTCAAAA GTTACC-3'; sense nt 7,823-7,842), and 10S (5'-GACT CCGTCGTGTGCTGCTC-3’; sense nt 7,649-7,668) with 10As (5'-CCTGGTCA TGGCCTCCGTGAA-3'; sense nt 8,681-8,701), and each pair of primers produces fragment 8, 9 and 10, covering NS4B, almost whole part of NS5A and NS5B, respectively. The PCR products were cloned using Mighty Cloning Reagent Set (Blunt End) (Takara Bio Inc., Japan) and sequenced.
Plasmid construction
pFK-Lu-JFH1 and pFK-Lu-JFH1/GND were generated from subgenomic replicon pSGR-JFH1 (AB114136.1) and pSGR-JFH1/GND (8) [both plasmids were kindly provided by Takaji Wakita (Department of Microbiology, Tokyo Metropolitan Institute for Neuroscience, Tokyo, Japan)], respectively, in which Neo gene was replaced by humanized Gaussia luciferase (hGLu) gene. In brief, an HCV replicon expressing hGLu was constructed by replacing Neo gene of plasmid pSGR-JFH1 with the luciferase gene from Gaussia princeps. The T7 promoter and the HCV 5' untranslated region (UTR) were amplified by PCR using JFH1-EcoR I (5'-GGAATTCTAATACGACTCACTATAG-3') and JFH1-hGL (5'-ACTTTGACTCCCATTTTGGTTTTTCTTTGAGG-3') as primers and pSGR-JFH1 as a template, while the hGLu gene was amplified by PCR using hGL-ATG (5'-ATGGGAGTCAAAGTTCTGTTTGC-3') and hGL-T (5'-TTAGTCACCACCGGCCCCCT-3') as primers and pRNAi-GL as a template (Takara Bio Inc., Japan). These two PCR products were used as templates for second round PCR to combine the 5’UTR with hGLu gene. The second round PCR product was digested with EcoR I and ligated with the linearized pSGR-JFH1 by digesting with EcoR I and Pme I. The newly generated pSGR-Lu-JFH1 and pSGR-Lu-JFH1/GND were double digested with Age I and EcoR V, respectively, and put into linearized pFK with same restriction enzyme sites.
The next step was to generate chimeric replicon of pFK -Lu-JFH1/0-37, pFK-Lu-JFH1/12-26 and pFK-Lu-JFH1/12-29, using pFK-Lu-JFH1 as template. Briefly, both clones of fragment 9 (clone 0w-37, 12w-26 and 12w-29) and pFK-Lu-JFH1 were digested with restriction enzyme Bae I, each relevant fragment was purified by gel extraction (QIAquick Gel Extraction Kit, Qiagen, Hilden, Germany). Chimeric replicon, where most part of wild type [Japanese fulminant hepatitis-1 (JFH1)] NS5A was replaced by patient’s HCV quasispecies sequence, was generated by in-fusion cloning method (Takara Bio Inc., Japan). The sequences of in-fusion primers used in the in-fusion cloning method are as below: forward primer: 5'-CCCTTCATCTCTTGTCAAAAGGGGTACAAGGGTGTGTGGGCCGGCACTGGTATCATGACCACACGCTGCCCTTG-3'; reverse primer: 5'-AGCCCCGGTCCAGGAGTATGACATGGA-3'.
RNA synthesis
We followed previously developed methods (9). In brief, we cut pFK-Lu-JFH1, pFK-Lu-JFH1/GND and chimeric replicon pFK –Lu-JFH1/0-37, pFK-Lu-JFH1/12-26 and pFK-Lu-JFH1/12-29 with Xba I, respectively, and treated them with mung bean nuclease (New England Biolabs Ltd., UK) to remove the 3'-protruding nucleotides. With this DNA, we synthesized HCV replicon RNA by using a MEGAscriptTM T7 kit (Applied Biosystems/Ambion, TX, USA). We treated the synthesized RNA with DNase I (Promega, WI, USA) at 37 ℃ for 15 min, and extracted it with acid phenol to remove remaining template DNA.
Cell culture and transfection
Huh-7.5.1 cells (9), which are highly permissive to HCV RNA replication, were maintained in Dulbecco’s modified Eagle’s medium (DMEM) (Sigma-Aldrich, MO, USA) supplemented with 10% fetal bovine serum (Invitrogen Corporation/Gibco, CA, USA), 100 µg/mL of kanamycin (Sigma), and non-essential amino acids (Invitrogen Corporation/Gibco). Each synthesized RNA was delivered to Huh-7.5.1 cells via Microporator MP-100 (Digital Bio, Korea). After 4 h, 100 mL of the supernatant was taken for assay, then we added 100 U/mL of IFN-a to the transfected cells and cultured in the incubator. After incubation with IFN-a for 24 h and 48 h, the cell supernatant was taken for assay, respectively. Total light output was detected by Turner Designs TD-20/ 20 Luminometer (Promega Co., USA).
Results
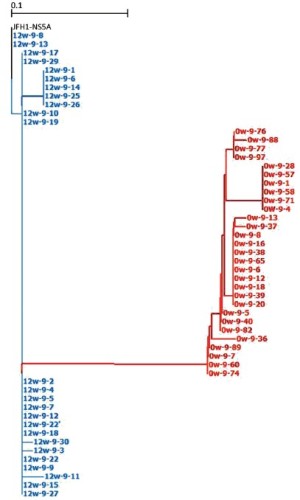
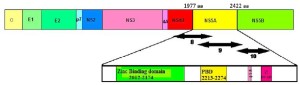
Evolution of HCV RNA after standard therapy
Regarding to standard therapy for HCV-infected patient, its efficacy depends on HCV genotype (5,10), although the mechanism underlying the different response among patients with different HCV genotypes is still unclear. However, this implies that viral genetic heterogeneity could affect, at least to some extent, the sensitivity to IFN-based therapy. So we amplified three different regions (Figure 1) of HCV RNA by RT-PCR and clone sequenced. As we can see in Figure 2, the pre- and post-treatment HCV sequences appeared to be almost uniform in three different regions, moreover, the quasispecies variation shrank to be further more simplified after 12 weeks of therapy.
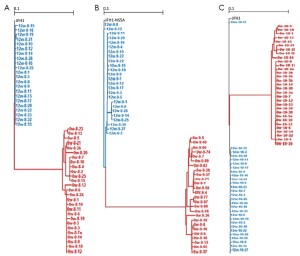
The IFN-sensitivity determining region (ISDR) has been discussed and was correlated with IFN responsiveness in HCV genotype 1b and 2a infection (11-14). But in our study, the population at the 12-week treatment in the region ISDR became more similar to the HCV-JFH1 (Figure 3), an IFN sensitive strain.
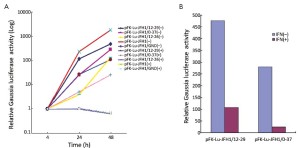
Chimeric subgenomic JFH1 replicon activity before and after IFN treatment
HCV resistance to IFN has been attributed, in part, to the function of the NS5A protein (13-16). To investigate how these NS5A changes on the influence of the virus replication and response to IFN, we constructed subgenomic JFH1 (wild type) and chimeric replicons (Figure 4). The Gaussia luciferase, inserted in replicon, possesses natural secretory signal and upon expression is secreted into the cell medium, so that cell supernatant can be used to evaluate each replicon’s activity. As shown in Figure 5, both chimeric replicons, pFK-Lu-JFH1/12-29 and pFK-Lu-JFH1/0-37 derived from post- and pre-treatment, respectively, exhibited higher replication ability, while another post-treatment-derived chimeric replicon, pFK-Lu-JFH1/12-26, did not replicate at all. Replication capacity of pFK-Lu-JFH1/12-29 was 4-fold powerful than pFK-Lu-JFH1/0-37, but its reaction efficiency to IFN-a was only 77%, much lower than pFK-Lu-JFH1/0-37 of 91%. So we compared these replicons’ ISDR region by amino acid alignment using GENETYX software (Figure 6), and found that pFK-Lu-JFH1/12-26 and pFK-Lu-JFH1/12-29 had only 3 and 1 amino acid differences with wild type JFH1, respectively, but pFK-Lu-JFH1/0-37 has 11s.
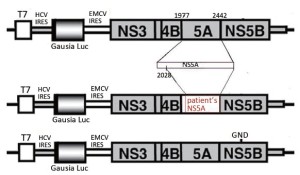

In addition, the loss of replication ability of pFK-Lu-JFH1/12-26 replicon attracted our interesting. Since NS5A’s zinc binding domain and PKR binding domain (PBD) are important for HCV replication (17-19), we performed amino acid sequence alignment in these regions (Figure 7), and found several pFK-Lu-JFH1/12-26 clone specific amino acid changes, such as S2047A, Y2094H, K2142E and F2144S in zinc binding domain (Figure 7A), and T2220S, S2223N, E2257A and C2274R in PBD (Figure 7B). These amino acid changes may closely relate to loss of HCV replication selected by IFN/RBV treatment in the HCV2a-infected patient. Further analysis using point mutation method for clarifying the role of these changes in the HCV life cycle is necessary.

Discussion
IFN/RBV combination therapy for HCV infected patients seems to be bound up with HCV genotype (5,10). Among different HCV genotypes, genotype 2 is more sensitive to the combination therapy, having a sustained viral response rate in 80% of patients in randomized controlled trials (4-6), but 20% of remanent patients still failed to response. To clarify the underlying mechanism, we analyzed the HCV sequences. Our data showed that the HCV population before and after treatment became almost uniform, and shrank to be further more simplified after 12 weeks of therapy, indicating during the course of the chronic infection, HCV population seemed to be adapted in some ways to the patient’s immune system, and IFN/RBV therapy may select IFN-resistant viruses. This simplified quasispecies may be completely eliminated by addition of other drugs with targets different from those of IFN/RBV.
In this study, the post-treatment population in ISDR region became more similar to HCV-JFH1 (Figures 3,6). In addition, as we can see from the chimeric replicon assay, although pFK-Lu-JFH1/12-29 has only one amino acid difference in ISDR region compared with IFN-sensitive JFH1 strain, its replication ability made up barely a quarter of wild-type ones, and the reaction efficiency to IFN-a was only 77%, much lower than wild type of 93%, and also lower than the pFK-Lu-JFH1/0-37 too, a clone owning 11 amino acid differences. These results were conflicting with those has been reported that ISDR was correlated with IFN responsiveness in HCV genotype 1b and 2a infection (11-14). The possible interpretations to this inconsistency include the following a few situations: (I) HCV in the 12-week sample is still moderately sensitive to IFN; (II) the ISDR is not correlated to IFN responsiveness at least in this case; (III) the small number of amino acid residues found in the 12-week sample but not in ISDR or near ISDR are important for resistance to IFN; and (IV) the amino acid change of Q2242R in pFK-Lu-JFH1/12-29 may has great meaning for HCV replication and susceptibility to IFN. Further analysis of the amino acid changes should be elucidated.
In conclusion, during the process of the chronic HCV infection, the viral population seems to be adapted to the patient’s immune system, and further to be selected by combination of IFN/RBV therapy, indicating quasispecies may completely eliminated by addition of other drugs with targets different from those of IFN. In addition, each distinct response of chimeric replicon to IFN is most likely related to amino acid changes in or near ISDR of NS5A during chronic infection and IFN/ RBV therapy.
Acknowledgements
We thank George Fu Gao at Institute of Microbiology, Chinese Academy of Science for helpful discussion.
Disclosure: The authors declare no conflict of interest.
References
- Sy T, Jamal MM. Epidemiology of hepatitis C virus (HCV) infection. Int J Med Sci 2006;3:41-6.
- Pawlotsky JM, Chevaliez S, McHutchison JG. The hepatitis C virus life cycle as a target for new antiviral therapies. Gastroenterology 2007;132:1979-98.
- Lavanchy D. Evolving epidemiology of hepatitis C virus. Clin Microbiol Infect 2011;17:107-15.
- Manns MP, McHutchison JG, Gordon SC, et al. Peginterferon alfa-2b plus ribavirin compared with interferon alfa-2b plus ribavirin for initial treatment of chronic hepatitis C: a randomised trial. Lancet 2001;358:958-65.
- Fried MW, Shiffman ML, Reddy KR, et al. Peginterferon alfa-2a plus ribavirin for chronic hepatitis C virus infection. N Engl J Med 2002;347:975-82.
- Arase Y, Suzuki Y, Suzuki F, et al. Efficacy of reduction therapy of natural human β-interferon and ribavirin in elderly patients with chronic hepatitis C, genotype 2 and high virus load. Hepatol Res 2012;42:750-6.
- Okamoto H, Sugiyama Y, Okada S, et al. Typing hepatitis C virus by polymerase chain reaction with type-specific primers: application to clinical surveys and tracing infectious sources. J Gen Virol 1992;73:673-9.
- Kato T, Date T, Miyamoto M, et al. Efficient replication of the genotype 2a hepatitis C virus subgenomic replicon. Gastroenterology 2003;125:1808-17.
- Zhong J, Gastaminza P, Cheng G, et al. Robust hepatitis C virus infection in vitro. Proc Natl Acad Sci USA 2005;102:9294-9.
- Sarasin-Filipowicz M. Interferon therapy of hepatitis C: molecular insights into success and failure. Swiss Med Wkly 2010;140:3-11.
- Enomoto N, Sakuma I, Asahina Y, et al. Mutations in the nonstructural protein 5A gene and response to interferon in patients with chronic hepatitis C virus 1b infection. N Engl J Med 1996;334:77-81.
- Murakami T, Enomoto N, Kurosaki M, et al. Mutations in nonstructural protein 5A gene and response to interferon in hepatitis C virus genotype 2 infection. Hepatology 1999;30:1045-53.
- EI-Shamy A, Shoji I, Kim SR, et al. Sequence heterogeneity in NS5A of hepatitis C virus genotypes 2a and 2b and clinical outcome of Pegylated-interferon/Ribavirin therapy. PLoS One 2012;7:e30513.
- Bouzgarrou N, Hassen E, Mahfoudh W, et al. NS5A (ISDR-V3) region genetic variability of Tunisian HCV-1b strains: Correlation with the response to the combined interferon/ribavirin therapy. J Med Virol 2009;81:2021-8.
- Gale M Jr, Kwieciszewski B, Dossett M, et al. Antiapoptotic and oncogenic potentials of hepatitis C virus are linked to interferon resistance by viral repression of the PKR protein kinase. J Virol 1999;73:6506-16.
- Kumthip K, Chusri P, Jilg N, et al. Hepatitis C virus NS5A disrupts STAT1 phosphorylation and suppresses type I interferon signaling. J Virol 2012;86:8581-91.
- Tellinghuisen TL, Marcotrigiano J, Gorbalenya AE, et al. The NS5A protein of hepatitis C virus is a zinc metalloprotein. J Biol Chem 2004;279:48576-87.
- Gale M Jr, Kwieciszewski B, Dossett M, et al. Antiapoptotic and oncogenic potentials of hepatitis C virus are linked to interferon resistance by viral repression of the PKR protein kinase. J Virol 1999;73:6506-16.
- Yokozaki S, Katano Y, Hayashi K, et al. Mutations in two PKR-binding domains in chronic hepatitis C of genotype 3a and correlation with viral loads and interferon responsiveness. J Med Virol 2011;83:1727-32.