Unusual presentation of cutaneous metastasis from bladder urothelial carcinoma
Introduction
Cutaneous metastasis from various primary internal malignancies is uncommon, and the incidence is reported to range from 0.2% to 10.4% (1). The incidence of cutaneous involvement by all urological malignancies is 1.1% to 2.5% (2). The kidney is the most common organ to serve as a source of metastasis to the skin (3). Bladder cancers are less likely to metastasize to the skin; the incidence in Taiwanese is only 0.22% (4). The clinical presentation of cutaneous metastases varies and can mimic many types of skin diseases. The most common clinical pictures of cutaneous metastases from genitourinary malignancies are infiltrated plaques or nodules (3). Due to patient and physician carelessness, misdiagnosis or delayed diagnosis is common. We report a patient who presented with multiple cutaneous metastases with an erysipelas-like appearance due to bladder urothelial carcinoma. The initial presentation was lymphedema of the right leg and suprapubic area.
Case report
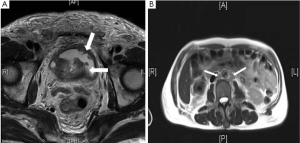
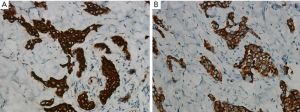
A 72-year-old previously healthy man presented with right leg edema and reddish swelling of the suprapubic area with a mildly painful sensation. Weak urine stream and urinary difficulty were also noted for several months but no gross hematuria was complained. He visited the cardiologist, and physical examination showed pitting edema of right leg and suprapubic area. Bladder tumor and right hydronephrosis were found incidentally by magnetic resonance angiography. Abdominal magnetic resonance imaging revealed multiple tumors in the bladder with muscle-layer invasion (Figure 1A) and pelvic and para-aortic lymph node enlargement (Figure 1B). The patient was considered to be in clinical stage T2N2M1. Chest radiography revealed a pulmonary mass, and peribronchial lesions were diagnosed by chest computed tomography. Cystoscopy showed multiple large papillary tumors on the bilateral lateral wall and trigone area of the bladder. Biopsy was performed. The pathological report revealed high-grade infiltration of urothelial carcinoma (Figure 2A). Consequently, the patient received chemotherapy with gemcitabin. Palm-sized erythematous plaques on the left flank area and suprapubic area were observed approximately 1 month after the patient received chemotherapy, but the patient ignored these lesions. Three months after chemotherapy, the patient complained of extensive painful erythematous plaques with an erysipelas-like appearance located on the suprapubic area, chest and abdomen (Figure 2B). Physical examination revealed warm erythematous plaques on the left chest, left flank, and suprapubic, prepuce and scrotal areas with tenderness. No fever or leukocytosis was noted. Excisional biopsies were obtained from the left chest and suprapubic areas. Histopathology showed tumor nests in the lymphatics with outgrowth into the surrounding dermis. The tumor cells were characterized by pleomorphic and hyperchromatic nuclei (Figure 2C). Immunohistochemistry revealed positivity for cytokeratin (CK) 7 (Figure 3A) and CK20 (Figure 3B). Ulcerative changes with pain in the prepuce and scrotal areas were noted 4 months after starting chemotherapy (Figure 4). No further treatment was performed for the cutaneous metastatic lesions due to the patient’s poor general condition. The patient received palliative treatment after 6 months of chemotherapy and died approximately 6 months after the cutaneous metastasis was diagnosed.

Discussion
The liver, lung, and bone are the most common sites of metastatic disease from genitourinary malignancies (5). Cutaneous involvement due to urological malignancy is uncommon; the incidence of cutaneous metastasis from bladder malignancies ranges from 0.84% to 3.60% (2). A large, 20-year, retrospective study in a Taiwanese population revealed only 2 patients with cutaneous metastases among 911 bladder and ureter cancer patients (4). The incidence is much lower in Taiwan than in Western countries. In our hospital, this patient is the first to present with cutaneous metastasis from bladder cancer. Clinical presentations of cutaneous metastasis are non-specific dermatological conditions; they often manifest as rapidly growing painless nodules (6). In urological cancer with cutaneous metastasis, the most common clinical picture is an infiltrated plaque or nodule (3). Ulcerated swelling, subcutaneous nodules, violaceous papules, and ulcerated plaques have been reported (1). A cutaneous erysipelas-like lesion, denoted as carcinoma erysipelatoides or erysipeloid-like carcinoma, has been reported in breast, lung, prostatic, thyroid and gastric cancer (7). There are only a limited number of case reports of cutaneous erysipeloid-like carcinoma that has metastasized from bladder carcinoma (7). This sort of clinical picture can mimic many other dermatological diseases, especially in patients receiving chemotherapy for skin infections. We report a case of cutaneous erysipelatoides carcinoma from bladder urothelial carcinoma who presented with painful erythematous plaques on the suprapubic, prepuce, and left chest areas.
There are many different pathophysiological manifestations of secondary lymphedema. Lymphatic filariasis is the most prevalent cause worldwide (8). In developed countries, the most common cause is malignancy (8). Lymphedema can be caused by malignant infiltration of lymph nodes or deeper lymphatics and superficial dermal lymphatics. The dermal lymphatics invade as lymphangitis carcinomatosa. Notably, lymphedema can be seen in the patients with cutaneous lymphangitis carcinomatosa because dermal lymphatics are infiltrated by tumor cells (9). The symptoms of lymphedema caused by cutaneous lymphangitis carcinomatosa are rapid onset and painful sensations (9). According to a previous report, the region of skin bordering the lymphedema displays erythematous changes characteristic of cutaneous lymphangitis carcinomatosa. These skin lesions can present clinically like erysipelas, but there is no true infection in these lesions. The skin consistency is more firm than that of true erysipelas (9). As in the presentation of our patient, the painful right leg and suprapubic swelling develop quickly. There are erythematous maculae in the suprapubic area. Therefore, we did not perform a skin biopsy during the early phase of the disease due to the surgeon’s limited experience with cutaneous metastasis. Chemotherapy was also performed due to the extensive metastasis in this patient. Because cutaneous metastasis can be the initial presentation of malignant disease, the diagnosis of cutaneous metastasis requires a high index of suspicion.
The prognosis of cancer cell metastasis to the skin presents a poor outcome (3). Among patients with bladder or renal cancer with cutaneous metastasis, most patients do not live longer than six months (3). Local excision, radiotherapy, chemotherapy, immunological and combination therapy have been reported in previous studies (10). Due to the poor outcomes of these patients, the treatment options are limited and primarily supportive in nature.
We report the case of a patient who initial presented with leg and suprapubic lymphedema caused by cancer infiltration in the dermal lymphatics. The unusual, painful erysipelas-like appearance of extensive metastatic lesions was noted. Although cutaneous metastasis is a rare dermatological condition, cutaneous metastasis should be included in the differential diagnosis of erysipelas-like skin lesions. Skin biopsy should be performed to prevent misdiagnosis. For the patients with urologic malignancies, we suggest that all urologists should increase attention to the physical examination of the skin because skin lesions can be the first sign of silent or recurrent urologic malignancies.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Nashan D, Müller ML, Braun-Falco M, et al. Cutaneous metastases of visceral tumours: a review. J Cancer Res Clin Oncol 2009;135:1-14. [PubMed]
- Block CA, Dahmoush L, Konety BR. Cutaneous metastases from transitional cell carcinoma of the bladder. Urology 2006;67:846.e15-7.
- Mueller TJ, Wu H, Greenberg RE, et al. Cutaneous metastases from genitourinary malignancies. Urology 2004;63:1021-6. [PubMed]
- Hu SC, Chen GS, Wu CS, et al. Rates of cutaneous metastases from different internal malignancies: experience from a Taiwanese medical center. J Am Acad Dermatol 2009;60:379-87. [PubMed]
- Babaian RJ, Johnson DE, Llamas L, et al. Metastases from transitional cell carcinoma of urinary bladder. Urology 1980;16:142-4. [PubMed]
- Hussein MR. Skin metastasis: a pathologist’s perspective. J Cutan Pathol 2010;37:e1-20. [PubMed]
- Zangrilli A, Saraceno R, Sarmati L, et al. Erysipeloid cutaneous metastasis from bladder carcinoma. Eur J Dermatol 2007;17:534-6. [PubMed]
- Warren AG, Brorson H, Borud LJ, et al. Lymphedema: a comprehensive review. Ann Plast Surg 2007;59:464-72. [PubMed]
- Damstra RJ, Jagtman EA, Steijlen PM. Cancer-related secondary lymphoedema due to cutaneous lymphangitis carcinomatosa: clinical presentations and review of literature. Eur J Cancer Care (Engl) 2010;19:669-75. [PubMed]
- Nashan D, Meiss F, Braun-Falco M, et al. Cutaneous metastases from internal malignancies. Dermatol Ther 2010;23:567-80. [PubMed]



