Radical gastrectomy for D2 distal gastric cancer
Patient’s information
The patient is a 56-year-old man who visited our hospital for “repeated epigastric pain for more than two months.” Physical examination showed nearly pale appearance; abdomen was soft and no mass palpable; left supraclavicular lymph node (-); and digital rectal examination (-). Gastroscopy revealed a bulging ulcerative lesion of the antrum at the lesion lesser curvature side, which had dirty appearance and was solid, fragile and prone to bleeding. Ultrasonic gastroscopy suggested myometrial invasion. Biopsy indicated adenocarcinoma. CT and MRI showed no obvious abnormalities. Therefore, the diagnosis of gastric cancer was definite for this patient. The preoperative staging was T3N0M0, and radical gastrectomy was considered (distal stomach, D2). The radical gastrectomy was performed under general anesthesia on April 21, 2013. The operation was uneventful, with intraoperative blood loss of about 250 mL. The length of operation was 180 minutes. Postoperative pathology suggested moderately differentiated adenocarcinoma of the “gastric antrum” with invasion to the serosa, and 2/35 of lymph nodes were positive. Postoperative staging: T3N1M0, stage III A. The patient was discharged 12 days after surgery and began chemotherapy (oxaliplatin + CF + 5-FU) at the department of oncology. The treatment course has been uneventful.
Surgical procedures
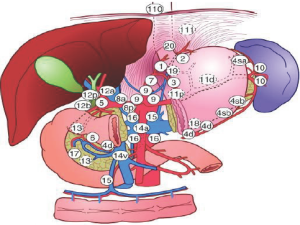
The main surgical instrument used in the operation is a Peng’s multifunction operative dissector (PMOD) invented by Professor Shuyou Peng, which enables scraping, suction, cutting, coagulation and other operations. In view of the important role of lymph node dissection in gastric cancer surgery (Figure 1), we have divided the procedure into three steps. The overall operation is conducted “from right to left and bottom to top” when denuding the lymph nodes for dissection and en bloc resection (Video 1).
Step one
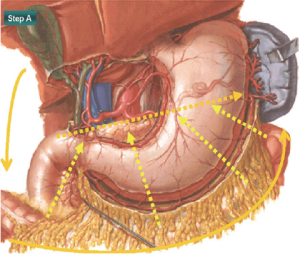
Gerota’s fascia and Kocher’s incision (Figure 2): the right renal fascia and the right fatty renal capsule are resected through a Kocher’s incision, and the right renal vein, inferior vena cava, right reproductive vein and abdominal aorta are gradually exposed. The head of the pancreas is then revealed (station 13), and the duodenum is freed during this process.
Treatment of the greater omentum and transverse mesocolon: the surgeon lifts the greater omentum with vascular forceps in the left hand, and the assistant retracts the transverse colon downward to form tension. With a PMOD in the right hand, the surgeon divides the greater omentum from the hepatic to the splenic region of the colon, and the anterior lobe of the transverse mesocolon through to the lower edge of the pancreas to reveal gastrocolic venous trunk, joined by the right colic vein and right gastroepiploic vein, and the superior mesenteric vein. The surrounding fat and lymphoid tissue is dissected (station 14), and the right gastroepiploic vein is separated and cut from its root. The surrounding fat and lymphoid tissue, as well as the pancreatic capsule, is lifted upwards together. The pancreatic capsule is separated from the middle to the right to expose the entire course of the gastroduodenal artery. The right gastroepiploic artery is then divided along this vessel and transected at the root. The surrounding fat and lymphoid tissue is dissected (station 6).
Step two
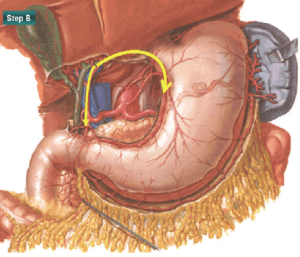
Treatment of the lesser omentum (Figure 3): after transection of the duodenum 2 cm inferior to the pylorus, the stomach is flipped upwards and cut longitudinally at the left edge of the common bile duct to expose the proper hepatic artery and portal vein. The separation is continued upwards to the bifurcation of the common bile duct and downwards to the common hepatic artery where the gastroduodenal artery emerges. The fat and lymphoid tissue anterior to and at the right side of the proper hepatic artery is dissected towards the left direction (station 12a), in which the root of the right gastric artery is revealed and transected. The surrounding lymph nodes as well as the entire right gastric artery are dissected towards the left (station 5), and the hepatogastric ligament is freed 1 cm beneath the liver upwards to the right diaphragm crus (stations 1 and 3).
Step three
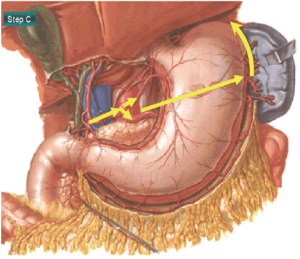
Treatment of the structures of the celiac trunk and the greater curvature region (Figure 4): using the proper hepatic artery as a landmark, the dissection is performed towards the celiac trunk to reveal the entire common hepatic artery, the initial region of the splenic artery and vein, and the left gastric artery and vein. The left gastric vessels are ligated at their roots, during which stations number 8a, 7, 9 and 11p are dissected. While dissecting stations 8 and 11p lymph nodes, feeding vessels from the pancreas often can be noted. With appropriate scraping and stripping with the PMOD, these small vessels can be rapidly separated and coagulated to ensure a clear surgical field while minimizing bleeding and avoiding potential injury to the pancreatic tissue due to redundant clamping. The stomach is flipped up to reveal the emerging point of the splenic artery from the celiac trunk. The fat and lymphoid tissue is then dissected (station 11) along the trunk of the splenic artery towards the splenic hilum. The gastrosplenic ligament is separated. During this step, it is necessary to ligate the left gastroepiploic artery and vein at their roots for dissection of station number 4sa lymph nodes.
Acknowledgements
Disclosure: The author declares no conflict of interest.