Safety and feasibility of video-assisted thoracoscopic surgery for stage IIIA lung cancer
Introduction
Lung cancer remains the leading cause of cancer death throughout the world, and most lung cancers are diagnosed in advanced stages (1). While stage IIIA lung cancer accounts for a high proportion, its treatment remains controversial (2). The use of video-assisted thoracoscopic surgery (VATS) for the treatment of lung cancer was first reported in 1992 (3-5). Compared with conventional thoracotomy, VATS is associated with smaller wounds, less postoperative pain, less damage to the chest muscle and respiratory function, lower postoperative levels of inflammatory factors in circulation related to injury, and higher immunity (6-11). However, only limited literatures have reported the application of VATS lobectomy for the treatment of stages II and III lung cancers (12-15). The impact of VATS lobectomy on the long-term survival of patients with stage IIIA lung cancer remains unclear (16).
The purpose of this study is to examine the feasibility of video-assisted thoracoscopic surgery (VATS) major pulmonary resection with systematic node dissection (SND) for clinical stage IIIA non-small cell lung cancer. Success is defined as VATS major pulmonary resection with SND without conversion. If success rate over 90%, VATS major pulmonary resection with SND is considered as feasible procedures for clinical stage IIIA non-small cell lung cancer. This study had been approved by the Ethics Committee of First Affiliated Hospital of Guangzhou Medical University, and all patients signed the informed consents. The clinical trial registration number of this study was NCT00862004.
Patients and Methods
Subject enrollment
The inclusion criteria were as follows: Histologically confirmed non-small cell lung cancer (Squamous, adenosquamous, large cell, or poorly differentiated) Stage IIIA (T1-3, N2, M0): N2 disease confirmed by any of the following: Mediastinoscopy; Bronchoscopy with fine-needle aspiration or esophagoscopy; or PET scan; ECOG performance status 0-1; From March 2009 to February 2010, a total of 51 patients with pre-operatively diagnosed stage IIIA NSCLC underwent VATS. All the patients underwent the total resection of the primary tumors and the systematic lymphadenectomy completely under the thoracoscope. The post-operative TNM staging was based on the seventh edition of International Association for the Study of Lung Cancer (IASLC) staging criteria. The baseline characteristics, treatment details, clinopathological data, and postoperative outcomes were recorded and analyzed.
Pre-operative preparation
The pre-operative preparation included detailed history-taking and physical examination, chest radiographic examination, thoracic and upper abdominal CT examinations, brain CT or MRI, pulmonary function tests, arterial blood gas analysis, ventilation/perfusion scan, and electrocardiography. Patients at risk for myocardial infarction also underwent echocardiography, thallium stress test, maximal oxygen uptake test, exercise test, and coronary angiography. Bronchoscopy was also performed before the surgery to clarify the stages of tumors inside the bronchi. If pre-operative CT showed lymph nodes sized >1.5 cm at the mediastinum or PET/CT dipicted mediastinal lymph nodes, mediastinoscopy or ultrasound bronchoscopy was performed for lymph node biopsy. Patients with PET/CT-identified pathologically confirmed metastases were enrolled in this study. For patients with symptoms and abnormal blood flow underwent further bone scans. For patients whose pre-operative lung function tests showed that they could not tolerate total pneumonectomy but the tumors were adhered to the main blood vessels, pulmonary artery angiography and remodeling were performed. For patients at high risk, right heart catheterization was performed to rule out pulmonary hypertension and prevent total pneumonectomy.
Operation
The procedures of VATS lobectomy has been described (17), which was similar to that reported by Shigemura et al. (16). Briefly, it was a purely endoscopic technique, with the operation completed fully based on the images displayed on the monitor. The operation hole was not retracted and sized about 3-5 cm (mean: 3.5 cm). Systematic lymph node dissection was performed upon the completion of lobectomy.
Post-operative care and follow up
After surgery, patients were advised to receive four to six cycles of platinum-based adjuvant chemotherapy. For N2 patients who had completed a thorough mediastinal lymph node dissection, not conventional adjuvant radiotherapy was conducted. In the case of enlarged lymph nodes during the follow-up period, adjuvant radiotherapy would be used for these patients. Postoperative follow-up data were obtained through post-operative revisits, imaging, and cancer patient registry. The incidences of complications and the mortality during the hospital and surgeries were recorded for each patient. After the surgery, chest CT was routinely performed every three months within the first post-operative year and every six months one year later.
Statistical analysis
Continuous variables used in descriptive statistics are presented as mean ± standard deviation, and categorical variables are presented using percentages. Statistical parameters included: age, gender, histological type, visceral pleura invasion, tumor size, lymph node metastasis, staging as per the 7th edition of TNM, and VATS lung resection type. The outcome indicators included the total number of the collected lymph nodes and the number of lymph node stations. Survival rates were calculated using the Kaplan-Meier curves. The survival time was calculated from surgery as a starting point, until death caused by cancer as an end point. The significance level is 0.05. All the statistical analyses were performed in the SPSS 15.0 software package.
Results
Patients’ characteristics
From March 2009 to February 2010, a total of 51 NSCLC patients who had undergone VATS pulmonary resection and met our inclusion criteria were enrolled in this study. The median follow-up period was 50.5 months. Of these 51 patients, 41 (80.4%) had N2 lymph node metastases. Among them 44 (86.3%) received pulmonary lobectomy and mediastinal lymph node dissection completely under the thoracoscope, 6 had their incisions extended to about 7 cm due to larger tumor sizes, and 1 had his surgery performed using a 12 cm small incision for handling the adhesions between lymph nodes and blood vessels (Table 1). The number of intra-operative lymph node dissection was 22.5±12.9, and the number of stations was 5.0±1.6. No patient was converted to conventional open thoracotomy.
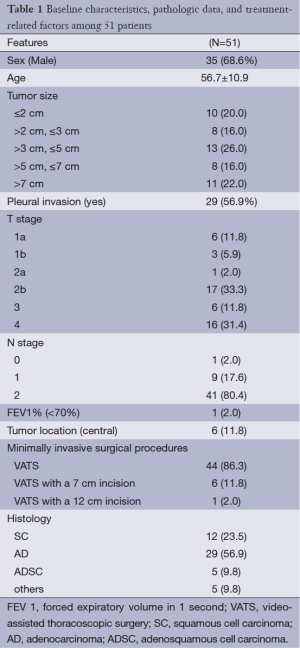
Full table
Complications and mortality
No intra-operative death was noted. One patient received a second surgery on the second post-operative day due to large drainage (>1,000 mL), and the postoperative recovery was satisfactory. In another patient whose daily drainage was larger than 500 mL, conservative treatment yielded satisfactory outcomes. Up to 45 patients (88.2%) did not suffer from any perioperative complication, and 6 (11.8%) experienced one or more complications (Table 2).
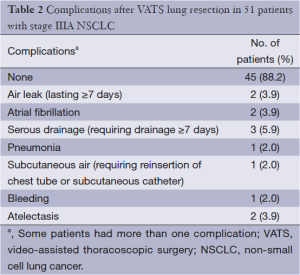
Full table
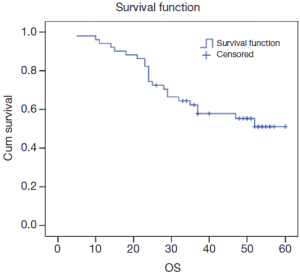
Overall survival
Among these patients, the average survival time was 44.0±2.6 months (median survival time could not be computed), and the 5-year survival rate was 51.1% (Figure 1).
Discussion
As a widely recognized technique, VATS lobectomy has been recommended by NCCN guidelines as the surgery of choice for early NSCLC. Our center has applied the VATS techniques for the radical resection of lung cancer since 1994, among which the thoracoscope-assisted small-incision operation was applied for the angioplasties in trachea, bronchus, and lung; the patients’ long-term survivals showed no significant difference when compared with the conventional open thoracotomy (18,19) However, the feasibility of surgical treatment for stage IIIA lung cancer with mediastinal lymph node metastasis (N2) remain controversial. Also, it is unclear whether the VATS technique can be applied for stage IIIA lung cancer with lymph node metastasis. McKenna et al. have successfully conducted VATS radical treatment for 1,100 patients with lung cancer (including post-operative pathologically confirmed stage IIIA lung cancer), without increase in complications (12). Watanabe et al. did a retrospective study aimed at determining the outcome of patients with cN0-pN2 NSCLC who underwent VATS major pulmonary resection with SND versus the outcome after major pulmonary resection with SND by open thoracotomy (15). It demonstrated that VATS major pulmonary resection with SND was a feasible approach to management of cN0-pN2 NSCLC without loss of curability. It was unnecessary to convert the VATS approach to thoracotomy in order to do SND even if pN2 disease is revealed during VATS major pulmonary resection. As part of multimodality therapeutic approachs, surgery offers a survival benefit for patients with resectable N2 NSCLC (17,20-24). Hennon et al. found that, when VATS was applied for the treatment of advanced lung cancer, it could smoothly and safely complete the expected tissue removal and lymphadenectomy (25). Our current study enrolled 51 patients with pre-operatively confirmed stage IIIA NSCLC, among whom the lobectomy and mediastinal lymph node dissection were successfully conducted. The intra-operative complications did not increase, and no patient was converted to conventional open thoracotomy. In a study with large sample size, after the surgery and multidisciplinary treatment for patients with stage IIIA NSCLC, the 5-year overall survival rates were 34.9% (26). In our cohort, the average survival time was (44.0±2.6) months, with the 5-year survival rate being 51.1%.
In conclusion, VATS radical treatment is a safe and feasible treatment for stage IIIA lung cancer.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Chen W, Zheng R, Zhang S, et al. Report of incidence and mortality in China cancer registries, 2009. Chin J Cancer Res 2013;25:10-21. [PubMed]
- Goldstraw P. New TNM classification: achievements and hurdles. Transl Lung Cancer Res 2013;2:264-72.
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Landreneau RJ, Hazelrigg SR, Ferson PF, et al. Thoracoscopic resection of 85 pulmonary lesions. Ann Thorac Surg 1992;54:415-9; discussion 419-20. [PubMed]
- Lewis RJ, Sisler GE, Caccavale RJ. Imaged thoracic lobectomy: should it be done? Ann Thorac Surg 1992;54:80-3. [PubMed]
- Cao C, Manganas C, Ang SC, et al. A meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomy. Ann Cardiothorac Surg 2012;1:16-23. [PubMed]
- Lacin T, Swanson S. Current costs of video-assisted thoracic surgery (VATS) lobectomy. J Thorac Dis 2013;5:S190-3. [PubMed]
- Shimizu K, Okita R, Nakata M. Clinical significance of the tumor microenvironment in non-small cell lung cancer. Ann Transl Med 2013;1:20.
- Liang Y, Wakelee HA. Adjuvant chemotherapy of completely resected early stage non-small cell lung cancer (NSCLC). Transl Lung Cancer 2013;2:403-10.
- Bar J, Urban D, Borshtein R, et al. EGFR mutation in lung cancer: tumor heterogeneity and the impact of chemotherapy. Chin Clin Oncol 2013;2:2.
- Sim YT, Poon FW. Imaging of solitary pulmonary nodule-a clinical review. Quant Imaging Med Surg 2013;3:316-26. [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [PubMed]
- Lewis RJ, Caccavale RJ, Sisler GE, et al. One hundred video-assisted thoracic surgical simultaneously stapled lobectomies without rib spreading. Ann Thorac Surg. 1997;63:1415-21; discussion 1421-2. [PubMed]
- Mahtabifard A, Fuller CB, McKenna RJ Jr. Video-assisted thoracic surgery sleeve lobectomy: a case series. Ann Thorac Surg 2008;85:S729-32. [PubMed]
- Watanabe A, Ohori S, Nakashima S, et al. Feasibility of video-assisted thoracoscopic surgery segmentectomy for selected peripheral lung carcinomas. Eur J Cardiothorac Surg 2009;35:775-80; discussion 780. [PubMed]
- Shigemura N, Hsin MK, Yim AP. Segmental rib resection for difficult cases of video-assisted thoracic surgery. J Thorac Cardiovasc Surg 2006;132:701-2. [PubMed]
- He J, Yang Y, Chen M. Lobectomy by video-assisted thoracoscopic surgery. Zhonghua Wai Ke Za Zhi 1996;34:76-8. [PubMed]
- He J, Shao W, Cao C, et al. Long-term outcome and cost-effectiveness of complete versus assisted video-assisted thoracic surgery for non-small cell lung cancer. J Surg Oncol 2011;104:162-8. [PubMed]
- He J, Shao W, Cao C, et al. Long-term outcome of hybrid surgical approach of video-assisted minithoracotomy sleeve lobectomy for non-small-cell lung cancer. Surg Endosc 2011;25:2509-15. [PubMed]
- Watanabe A, Mishina T, Ohori S, et al. Is video-assisted thoracoscopic surgery a feasible approach for clinical N0 and postoperatively pathological N2 non-small cell lung cancer? Eur J Cardiothorac Surg 2008;33:812-8. [PubMed]
- Walker WS, Codispoti M, Soon SY, et al. Long-term outcomes following VATS lobectomy for non-small cell bronchogenic carcinoma. Eur J Cardiothorac Surg 2003;23:397-402. [PubMed]
- Roviaro G, Varoli F, Vergani C, et al. Long-term survival after videothoracoscopic lobectomy for stage I lung cancer. Chest 2004;126:725-32. [PubMed]
- Congregado M, Merchan RJ, Gallardo G, et al. Video-assisted thoracic surgery (VATS) lobectomy: 13 years' experience. Surg Endosc 2008;22:1852-7. [PubMed]
- Bakir M, Fraser S, Routledge T, et al. Is surgery indicated in patients with stage IIIa lung cancer and mediastinal nodal involvement? Interact Cardiovasc Thorac Surg 2011;13:303-10. [PubMed]
- Hennon M, Sahai RK, Yendamuri S, et al. Safety of thoracoscopic lobectomy in locally advanced lung cancer. Ann Surg Oncol 2011;18:3732-6. [PubMed]
- Liang W, Shao W, Jiang G, et al. Chinese multi-institutional registry (CMIR) for resected non-small cell lung cancer: survival analysis of 5,853 cases. J Thorac Dis 2013;5:726-9. [PubMed]


